The EEOICPA provides eligible individuals who have contracted a serious illness as a result of exposure to radiation or other toxic substances with monetary compensation as well as access to medical coverage. To ensure that covered parties are able to receive the care that they deserve, each eligible person receives a medical identification card that is presented at the time of treatment. For this reason, Medicaid and or private insurance carriers do not need to be billed for medical expenses related to covered illnesses.
Medical Benefits Identification Cards
Once a covered employee has been awarded medical benefits, he or she receives a medical benefits identification card that includes certain information, including:
- The employee’s name;
- The diagnosis code of the accepted conditions;
- A statement explaining that the card carrier does not owe a co-pay or deductible expense;
- The address where medical bills must be sent;
- A toll-free telephone number for medical billing questions; and
- A ten digit number for internet access to the card carrier’s medical billing file, which allows the holder to check the status of his or her medical bills.
Once an employee receives this card, he or she can present it at the time of treatment to the medical provider who can then bill the appropriate entity. The cardholder must also provide his or her Social Security number to the medical provider at this time. Holders can even use these cards to obtain reimbursement for out-of-pocket medical expenses that were incurred before the claim was accepted.
What Medical Benefits are Provided?
Under EEOICPA, those who have had their claims approved are eligible to receive the following medical benefits:
- Reasonable and customary medical care, such as doctor’s visits, consultations, and treatment;
- In-patient and out-patient hospital charges;
- Diagnostic laboratory and radiological testing;
- Medical equipment;
- Prescription drugs;
- Ambulance services; and
- Travel costs directly associated with treating a covered illness.
Any expenses related to these services can and should be billed to EEOICPA’s medical bill payment agent in London, Kentucky by the medical provider. If the medical provider is enrolled in the program, EEOICPA will pay him or her directly. If a medical provider is not enrolled in the program, he or she can seek enrollment assistance by calling the toll free number on the back of the patient’s medical benefits identification card. Patients can also choose to pay for the service out of pocket and then seek reimbursement from EEOICPA at a later date.
Card holders who obtain treatment for an illness that is unrelated to their claim, however, will not have their expenses covered by EEOICPA. These are the only costs that may be billed to the employee’s insurer or Medicaid.
Contact a Home Health Care Professional Today
If you or a loved one is covered by EEOICPA and you have questions about the kind of home medical care you are entitled to, please contact a member of our experienced home health care team at United Energy Workers Healthcare and Four Corners Health Care. We are prepared to help you today.[/vc_column_text]
Who We Serve
Do you have this card?
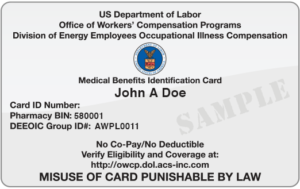
If you already have this card, then you are already approved to receive no-cost medical benefits! Call us to get started today.
In order to be eligible for EEOICPA/RECA benefits, an individual must have been employed at a covered Department of Energy facility, an approved atomic weapons facility, or at a permitted beryllium vendor. An individual must also have one of the covered conditions as a result of exposure to radiation, beryllium, or silica while employed at an accepted facility. In addition, uranium miners, millers, and ore transporters are eligible for benefits if they develop an illness as a result of exposure to toxic substances (such as radiation, chemicals, solvents, acids, and metals) and worked at a facility covered under RECA. Eligibility requirements vary by location and condition.